Receiving a cancer diagnosis is a life-altering moment, filled with uncertainty and questions. If you or a loved one are facing this journey with testicular cancer, it’s important to know one thing right away: it is one of the most treatable and curable forms of cancer. With early detection and modern medical care, the prognosis is overwhelmingly positive.
This guide is here to walk you through every step of the testicular cancer treatment in Jaipur. We will cover everything from understanding the initial signs to navigating treatment options and embracing life after recovery. Think of this as your comprehensive resource, designed to provide clarity, confidence, and hope as you take the next steps toward a healthy future. Jaipur stands as a center for excellence in medical care, offering advanced technology and experienced specialists to guide you.
Understanding Testicular Cancer and Your Options in Jaipur
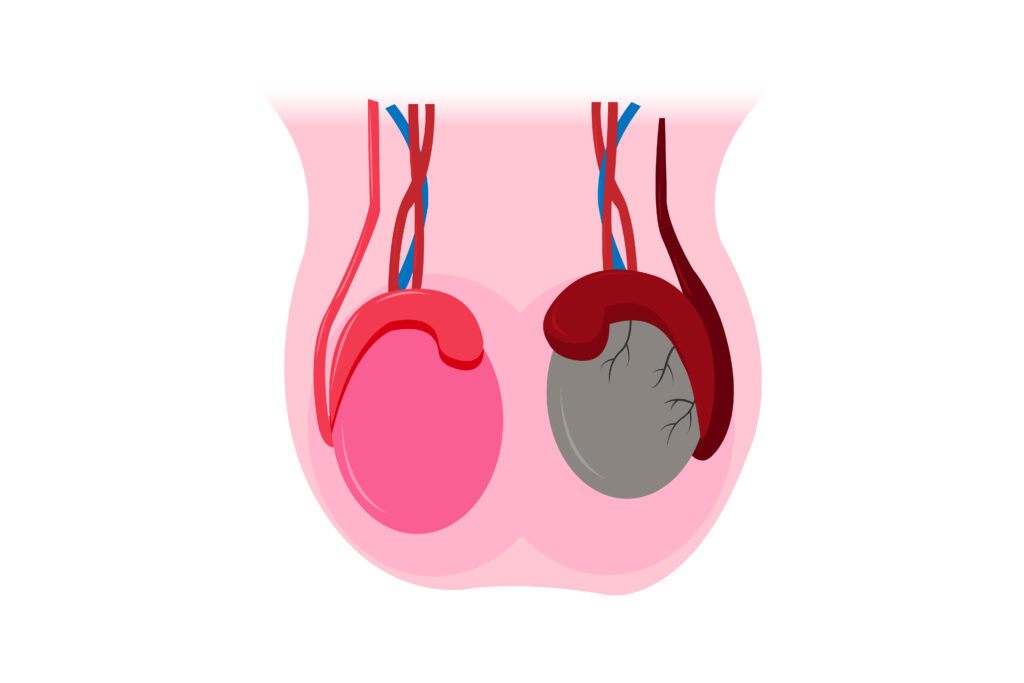
Testicular cancer develops in the testicles, which are part of the male reproductive system. These organs produce male hormones like testosterone and sperm. The cancer typically begins in the germ cells, which are the cells that produce immature sperm.
While the thought of cancer is scary, the statistics for testicular cancer are very encouraging. The cure rate is over 95%, and for men whose cancer is found before it spreads, the survival rate is nearly 99%. This is why awareness and proactive health checks are so important.
Jaipur has emerged as a leading hub for high-quality, accessible medical care in India. The city’s hospitals are equipped with state-of-the-art diagnostic tools, advanced surgical facilities, and dedicated oncology departments staffed by experts in urological cancers. This means you can access world-class testicular cancer treatment in Jaipur without the need for extensive travel.
The Two Main Types of Testicular Cancer: Seminoma vs. Non-Seminoma
When you receive a diagnosis, one of the first things your doctor will determine is the type of testicular cancer you have. This classification is vital because it directly influences your treatment plan. Nearly all testicular cancers are germ cell tumors, which are divided into two main categories: seminomas and non-seminomas.
Seminomas
Seminomas tend to grow and spread more slowly than non-seminomas. They are very sensitive to radiation therapy and chemotherapy, which makes treatment highly effective. There are two subtypes:
- Classical Seminoma: This is the most common type, accounting for over 95% of seminoma cases, and usually affects men between 25 and 45.
- Spermatocytic Seminoma: A rarer type that tends to affect older men and has an even better prognosis as it rarely spreads.
Non-Seminomas
Non-seminomas typically occur in men in their late teens to early 30s. This category is made up of several subtypes, and tumors are often a mix of these different cell types. They tend to grow more quickly than seminomas. The main subtypes include:
- Embryonal Carcinoma: A fast-growing type.
- Yolk Sac Carcinoma: The most common type in young boys.
- Choriocarcinoma: A very rare and aggressive type.
- Teratoma: These tumors can be complex, containing different types of tissue.
A pathologist will examine the tumor tissue after surgery to confirm the exact type, which is a crucial step in planning your testicular cancer treatment.
Early Warning Signs & How to Perform a Testicular Self-Exam
Early detection is your most powerful tool. The most common sign of testicular cancer is a lump or swelling on a testicle. That’s why performing a monthly testicular self-exam (TSE) is so important.
Key Symptoms to Watch For:
- A painless lump or swelling on either testicle.
- A feeling of heaviness in the scrotum.
- A dull ache or pain in the lower abdomen or groin.
- A sudden collection of fluid in the scrotum.
- Pain or discomfort in a testicle or the scrotum.
It’s important to remember that other conditions can cause these symptoms. However, you should never ignore them.
How to Perform a Testicular Self-Exam (TSE): A Step-by-Step Guide
- Choose the Right Time: The best time is during or after a warm bath or shower, when the scrotal skin is relaxed.
- Examine Each Testicle: Use both hands to examine one testicle at a time. Place your index and middle fingers under the testicle with your thumbs on top.
- Roll Gently: Roll the testicle gently between your thumbs and fingers. You are feeling for any hard lumps, smooth rounded bumps, or changes in the size, shape, or consistency of the testicle.
- Know Your Body: It’s normal for one testicle to be slightly larger than the other. At the back of each testicle is the epididymis, a soft, rope-like tube that stores sperm. Get to know how it feels so you don’t mistake it for a lump.
If you find anything unusual, schedule an appointment with a urologist right away.
The Diagnostic Pathway: What to Expect in Jaipur Hospitals
If you’ve found a lump or have other symptoms, your doctor will follow a clear pathway to get a diagnosis. In Jaipur, hospitals are equipped with the latest technology to ensure this process is quick and accurate.
- Physical Examination: Your doctor will examine your testicles for lumps, swelling, or tenderness.
- Scrotal Ultrasound: This is the most common next step. An ultrasound is a painless imaging test that uses sound waves to create a picture of the inside of your scrotum. It can determine if a lump is solid (which could be cancer) or filled with fluid (likely a cyst).
- Blood Tests for Tumor Markers: Your doctor will order blood tests to check for specific proteins called tumor markers. The main markers for testicular cancer are Alpha-fetoprotein (AFP), Beta-human chorionic gonadotropin (beta-hCG), and Lactate dehydrogenase (LDH). Elevated levels can indicate testicular cancer.
- Radical Inguinal Orchiectomy: If the ultrasound and blood tests suggest cancer, the standard procedure is a radical inguinal orchiectomy. This is surgery to remove the entire testicle through an incision in the groin. This surgery serves two purposes: it provides the tissue for a definitive biopsy to confirm the cancer type, and it is the primary treatment for removing the localized tumor.
Staging Testicular Cancer: Understanding the Extent of the Disease
Once cancer is confirmed, the next step is staging. Cancer staging is the process of finding out how far the cancer has spread. This is crucial for determining the best treatment plan and understanding the prognosis. The system used is the TNM system, which stands for Tumor, Node, and Metastasis.
- Stage I: The cancer is confined to the testicle.
- Stage II: The cancer has spread to the lymph nodes in the abdomen (the retroperitoneal lymph nodes).
- Stage III: The cancer has spread to distant parts of the body, such as the lungs, liver, or brain, or to distant lymph nodes.
To determine the stage, your doctor will order a CT scan of your chest, abdomen, and pelvis. This imaging helps them see if the cancer has spread to lymph nodes or other organs.
Surgical Treatment: The Cornerstone of Curing Testicular Cancer
Surgery is the primary and most essential part of testicular cancer treatment in Jaipur.
Radical Inguinal Orchiectomy
As mentioned, this surgery is the first step for nearly every patient. A uro-oncologist, a surgeon specializing in urological cancers, performs the procedure. The incision is made in the groin, not on the scrotum, to prevent any risk of cancer cells spreading into the lymphatic channels of the scrotum. The entire spermatic cord is also removed along with the testicle. This is a highly effective procedure for removing the primary tumor.
Retroperitoneal Lymph Node Dissection (RPLND)
For some patients with non-seminomas, a second, more complex surgery called a Retroperitoneal Lymph Node Dissection (RPLND) may be recommended. This surgery involves removing the lymph nodes at the back of the abdomen where testicular cancer often spreads first. It can be done to treat cancer that has already spread or as a preventive measure in high-risk cases. This is a major operation that should only be performed by highly experienced surgeons.
Chemotherapy Regimens for Testicular Cancer in Jaipur
Chemotherapy uses powerful drugs to kill cancer cells throughout the body. It is often used after surgery (as an “adjuvant” therapy) to eliminate any remaining cancer cells and reduce the risk of recurrence, or as the main treatment for cancer that has spread.
The most common chemotherapy regimen for testicular cancer is BEP, which stands for:
- Bleomycin
- Etoposide
- Platinol (a brand name for Cisplatin)
These drugs are administered intravenously (IV) in cycles, with a period of treatment followed by a period of rest to allow your body to recover. A medical oncologist in Jaipur will manage your chemotherapy, tailoring the number of cycles to the stage and type of your cancer.
The Role of Radiation Therapy (Radiotherapy)
Radiation therapy uses high-energy X-rays to destroy cancer cells. For testicular cancer, its use is very specific. It is highly effective for treating seminomas.
Radiation is most commonly used as an adjuvant therapy for Stage I and Stage II seminomas after surgery. The radiation is aimed at the retroperitoneal lymph nodes in the abdomen to kill any cancer cells that may have spread there. Modern cancer centers in Jaipur use advanced linear accelerators (LINAC) to deliver this radiation with incredible precision, minimizing damage to surrounding healthy tissue.
How to Choose the Best Hospital and Doctor in Jaipur
Choosing your medical team is one of the most important decisions you will make. Here are some criteria to help you find the best hospital for testicular cancer in Jaipur:
- Accreditation: Look for hospitals with NABH (National Accreditation Board for Hospitals & Healthcare Providers) accreditation, which signifies high standards of patient care and safety.
- Specialized Department: Choose a hospital with a dedicated uro-oncology department.
- Multidisciplinary Tumor Board: The best cancer centers have a tumor board where surgeons, medical oncologists, and radiation oncologists meet to discuss patient cases and create a unified treatment plan.
- Doctor’s Experience: Ask your doctor about their experience with testicular cancer. A top testicular cancer doctor in Jaipur will have treated many cases and be familiar with the latest treatment protocols.
- Patient Reviews: Look for testimonials and reviews from other patients.
- Seek a Second Opinion: It is always wise to get a second opinion to feel confident in your diagnosis and treatment plan.
Navigating the Cost of Treatment and Insurance in Jaipur
The cost of testicular cancer treatment in Jaipur can vary widely depending on the hospital (private vs. government), the stage of the cancer, and the specific treatments required.
Here’s a general breakdown of potential expenses:
- Diagnostics: Ultrasounds, blood tests, and CT scans.
- Surgery: Surgeon’s fees, hospital stay, and operating room charges.
- Chemotherapy/Radiation: Cost of drugs, number of cycles/sessions.
- Follow-up Care: Future scans and appointments.
Most health insurance plans in India cover cancer treatment. Contact your insurance provider early to understand your coverage. Many hospitals in Jaipur have insurance desks and financial counselors who can help you with cashless claims and navigating the paperwork.
Fertility Preservation: Planning for a Future Family
This is a critical topic that must be addressed before starting certain treatments. Both chemotherapy and radiation can permanently affect sperm production and cause infertility.
The best way to preserve your ability to have biological children is through sperm banking (cryopreservation). This involves collecting and freezing semen samples for future use. This simple and effective procedure should be done after surgery but before you begin any chemotherapy or radiation.
Talk to your oncologist about this right away. They can refer you to a fertility clinic in Jaipur. Making time for sperm banking is an investment in your future.
Managing Treatment Side Effects: A Practical Guide
Cancer treatments are powerful, and they can cause side effects. Your oncology team will provide supportive care to help manage them.
Short-Term Side Effects (from Chemo/Radiation)
- Nausea and Vomiting: Anti-nausea medications are very effective.
- Fatigue: This is very common. Listen to your body and rest when you need to.
- Hair Loss: Hair typically begins to grow back a few months after treatment ends.
Potential Long-Term Side Effects
- Neuropathy: Numbness or tingling in the hands and feet from certain chemo drugs.
- Hearing Changes: Ringing in the ears (tinnitus) can occur.
Communicate openly with your medical team about any side effects you experience. They are there to help you maintain the best possible quality of life during treatment.
Life After Treatment: Surveillance, Recurrence, and Survivorship
After you complete your treatment, you enter the next important phase: surveillance. This is a structured follow-up plan to monitor your health and check for any signs of the cancer returning (recurrence). This careful monitoring is a key reason for the high cure rate.
A typical surveillance schedule includes:
- Regular Physical Exams
- Blood Tests for Tumor Markers
- CT Scans of the abdomen and chest
These appointments will be frequent at first and become less frequent over time. Adhering to this follow-up for testicular cancer schedule is essential for your long-term health and peace of mind.
Psychological and Emotional Support During and After Treatment
A cancer diagnosis impacts more than just your physical health. It’s normal to feel anxiety, fear, or depression. Addressing your mental and emotional well-being is a vital part of your recovery.
Many hospitals in Jaipur have onco-psychologists or counselors who specialize in helping cancer patients. Support groups, either online or in-person, can also be incredibly helpful. Connecting with others who have been through a similar experience can reduce feelings of isolation. Don’t hesitate to seek emotional support for cancer patients—it is a sign of strength.
Considering a Testicular Prosthesis: Options and Decision
After an orchiectomy, some men are concerned about their physical appearance. A testicular prosthesis is a cosmetic option to restore the natural look of the scrotum. The prosthesis is a saline-filled implant that is matched to the size and shape of the remaining testicle.
The decision to get an implant is a personal one. It can be placed during the initial surgery or in a separate procedure later. Discuss the pros and cons with your urologist to decide if it is the right choice for you.
Your Path to a Healthy Future Starts in Jaipur
Navigating a diagnosis of testicular cancer can be overwhelming, but you are not alone. From the first diagnosis to long-term survivorship, Jaipur offers a complete ecosystem of expert medical care, advanced technology, and compassionate support.
The key takeaways are clear: testicular cancer is highly curable, early detection is paramount, and a clear treatment path is available to you. The most powerful tool you have is taking action.
If you have noticed any symptoms or have any concerns, do not delay. Consult a specialist. Your proactive step today is the beginning of your journey back to health and a bright, cancer-free future.